Periodontology
by Dr. Sofia Bettini
Periodontology is the branch of dentistry that deals with the treatment of the periodontium, i.e. the supporting tissue of the tooth, composed of: alveolar bone, periodontal ligament, root cement and gingiva.
Periodontal disease
Periodontal disease is an inflammation of the periodontium due to the action of bacteria present in plaque and tartar. The main causes are: poor or inaccurate oral hygiene, tartar accumulation, smoking, family predisposition. It can be associated with certain systemic diseases such as diabetes. As a chronic condition, periodontal disease usually does not cause pain. In some cases, the disease can become acute, with the formation of a periodontal abscess, intra- and/or extra-oral pain and swelling.
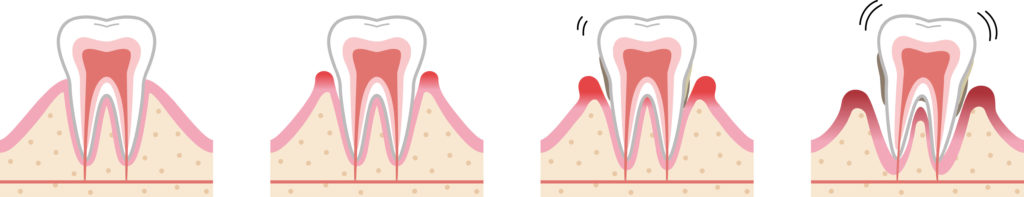
Gingivitis is the initial form of periodontal disease, involving only the gum. The symptoms of gingivitis are redness, swelling and bleeding of the gums (during home or spontaneous oral hygiene manoeuvres). If left untreated, gingivitis can progress and evolve into periodontitis.
Periodontitis (also known as pyorrhea) is a more advanced form of inflammation, which causes resorption of the supporting alveolar bone of the tooth with the formation of periodontal pockets. In addition to redness, swelling, and bleeding of the gums, the symptoms of periodontitis are bad breath, bad taste, “longer” teeth, mobility or displacement of the teeth.
Lack of tooth support tissue can cause tooth loss. To avoid or limit the loss of teeth, it is important to treat gingivitis and periodontitis correctly.
During the specialist visit, a periodontal chart will be compiled, and intraoral radiographs will be taken. The diagnosis of periodontal disease is made by observation and analysis of clinical and radiographic signs and symptoms.
After the diagnosis of periodontal disease, the first stage of treatment includes the elimination of risk factors. In collaboration with the dental hygienist, the patient will be instructed in the correct home oral hygiene maneuvers and the use of a toothbrush and interdental brush to avoid the accumulation of plaque and tartar. Giving up smoking is also a very important aspect of reducing the progression of periodontal disease. It is then necessary to perform root planing, to remove the tartar accumulated above and below the gingival margin with manual and ultrasonic instruments. In some cases, non-surgical therapy is sufficient to stabilize the disease.
In other cases, however, a second phase of treatment, which includes surgical therapy, is necessary. The goal is to regulate the supporting tissue of the teeth, allow the patient to perform effective home hygiene, avoiding the accumulation of tartar, and in some cases regenerate part of the lost alveolar bone. Surgical therapy is performed under local anesthesia, involves antibiotic coverage, and requires 1-2 weeks of rest after surgery. In the first post-operative days it is possible to have some pain, which can be controlled with standard anti-inflammatories.
At the end of the treatment, the patient is given a maintenance programme to follow at home and is monitored regularly both by the dentist and the dental hygienist.
Receding gums
Gum recession is a displacement of the gingival margin, with exposure of the underlying tooth root. The main causes are incorrect and/or aggressive oral hygiene manoeuvres, the accumulation of plaque and tartar, poorly positioned dental elements, lip or tongue piercings, lip frenulum, genetic predisposition (thin gums). Gum recession can be associated with hypersensitivity to cold food and drink, aesthetic problems (longer tooth), difficulty in home oral hygiene. The exposed tooth root is also at high risk of developing tooth decay.

Treatment of gum recession involves periodontal plastic surgery to return the gum to its initial position. To reduce the risk of recurrence, the gum is also thickened with a graft, usually taken from the patient’s palate. Sometimes gum recession is associated with an abrasion of the tooth collar – in these cases, in addition to the surgical procedure, a composite filling must also be performed to reconstruct the collar.
Surgical therapy is performed under local anesthesia, involves antibiotic coverage and requires 2 weeks of rest after surgery. In the first post-operative days it is possible to have some pain, which can be controlled with standard anti-inflammatories.
At the end of the treatment, the patient is given a maintenance programme to follow at home and is monitored regularly both by the dentist and the dental hygienist.
Clinical corona elongation
The portion of the tooth visible in the oral cavity is called a “clinical crown”.
This technique involves the removal of a small portion of the gum and alveolar bone, in order to expose a portion of the tooth previously covered, making it visible and usable to reconstruct or cover the tooth. The surgical procedure is performed under local anesthesia, involves antibiotic coverage, and requires 1-2 weeks of rest after surgery. In the first few post-operative days it is possible to have some pain, which can be controlled with standard anti-inflammatories.
After the operation, hypersensitivity to cold may appear in the portion of the tooth newly exposed to the oral cavity, which disappears spontaneously within a few weeks or by using special desensitizing products.
Approximately 2 weeks after the surgical procedure, the patient will be able to proceed with the reconstruction or re-covering of the affected tooth.

